The Definitive Guide To Wisdom Teeth Removal
This is the ultimate guide to wisdom teeth and wisdom teeth removal.
This is not content you will find anywhere else on the Internet. This content is written and produced by Dr. Navid Senehi, DDS. MD. and founder of Facial & Oral Surgery Institute in Woodland Hills, CA.
Dr. Navid Senehi is a nationally known oral surgeon who is regarded amongst his peers and patients as The Third Molar Master. He is an expert on oral and maxillofacial surgery including wisdom teeth removal.
So if you're looking to learn as much as you can about wisdom teeth and wisdom teeth removal, you'll love this guide.
Let's dive right in.

What You Should Know About Wisdom Teeth
The wisdom of wisdom teeth removal
Wisdom teeth removal is a traditional practice verging on a rite of passage for many Americans. The procedure is so common, in fact, that in any given year over 10 million wisdom teeth, or third molars, are extracted from patients in the United States alone.
That’s a lot of teeth.
Conventional wisdom, however, on the efficacy and necessity of removing these troublesome molars has faced some questions in recent times.
What are ‘wisdom teeth’ and why do we have wisdom teeth?
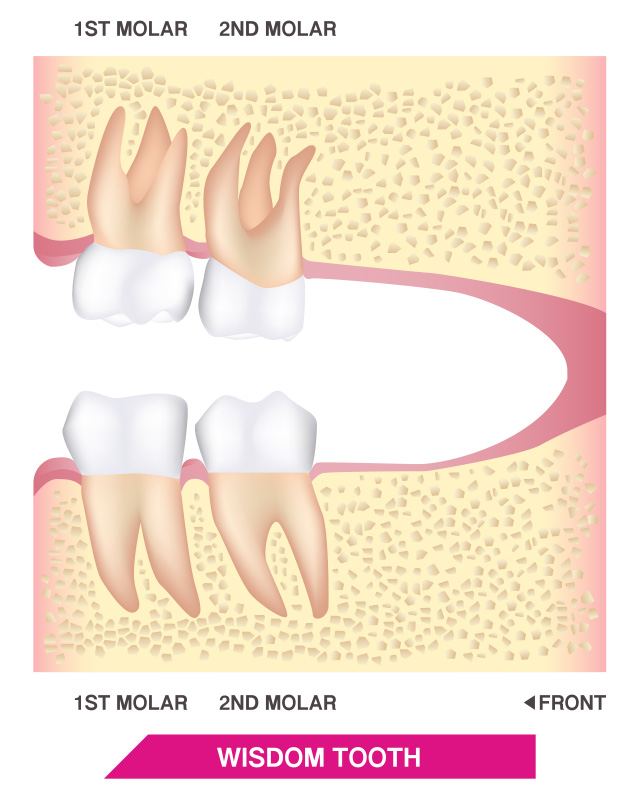
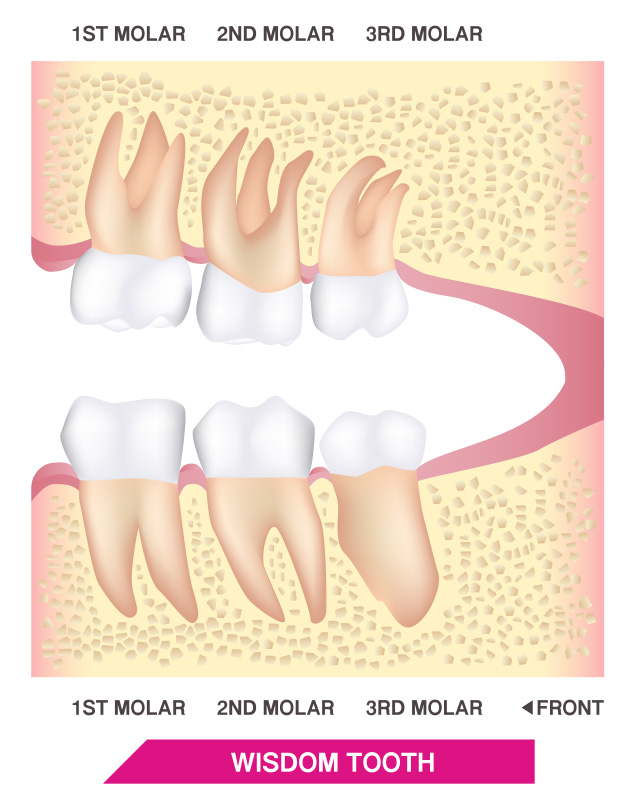
Wisdom teeth, also known as third molars, are the third and final set of molars located at the very back of a person’s mouth. Most people have two sets of wisdom teeth - two teeth in the upper jaw and two in the lower - for a total of four wisdom teeth. Unfortunately, for the vast majority of modern human beings, these extra molars are nothing but vestigial teeth from a far distant past. For most of us, they are nothing but trouble.
Once upon a time, our strong-jawed hunter-gatherer ancestors relied on these change molars to grind up tough roots, hard nuts, and sinewy meats. Once we learned how to farm staple grains such as wheat, barley, and rice, and discovered that cooking food was a great idea, our need for such strong jaws and extra teeth disappeared. Our mouths have been shrinking ever since resulting in jawbones that simply don’t have enough space to accommodate all our teeth.
Wisdom Teeth Removal FAQ
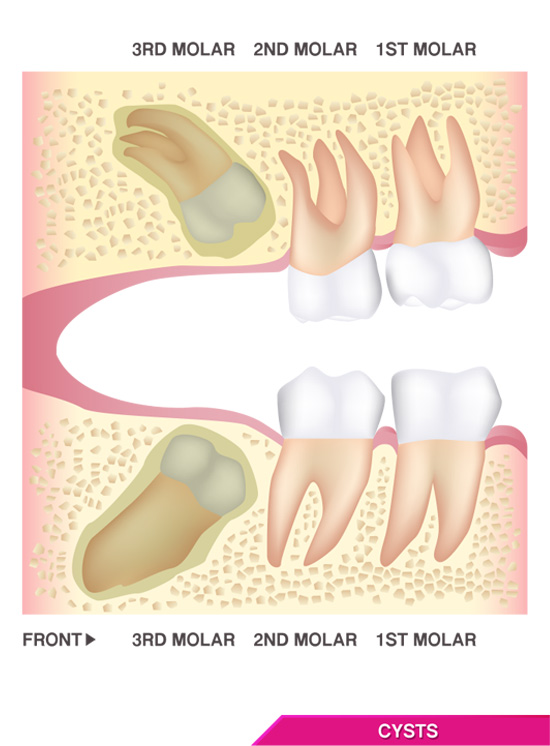
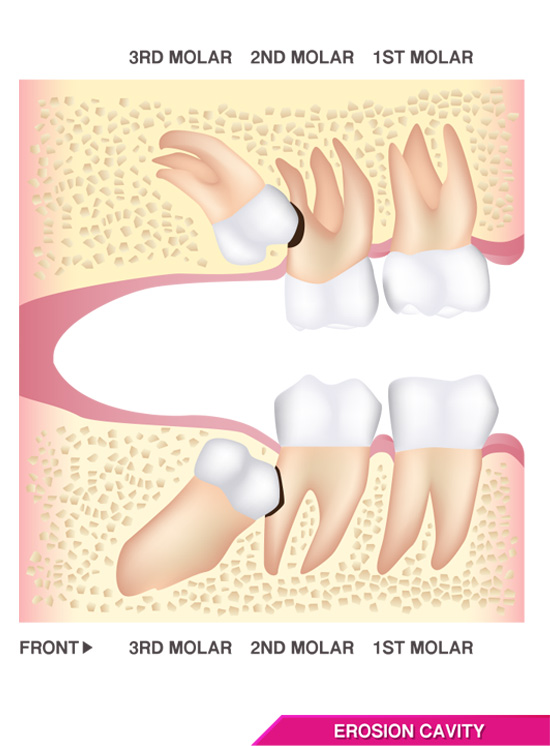
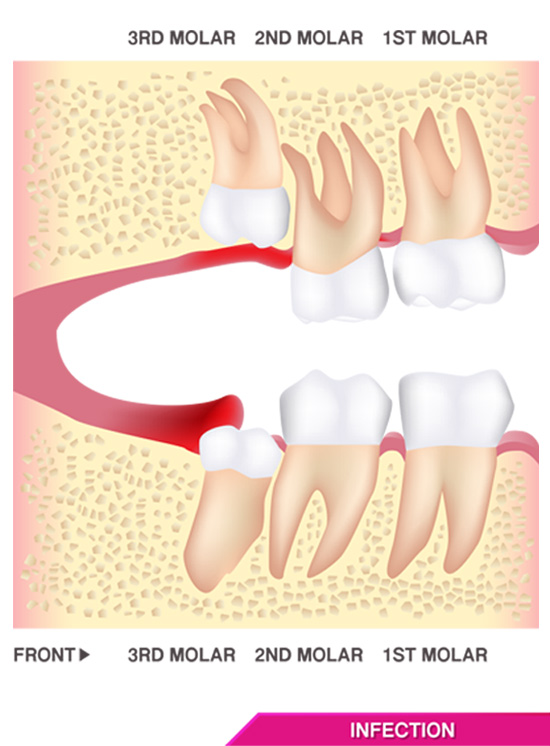
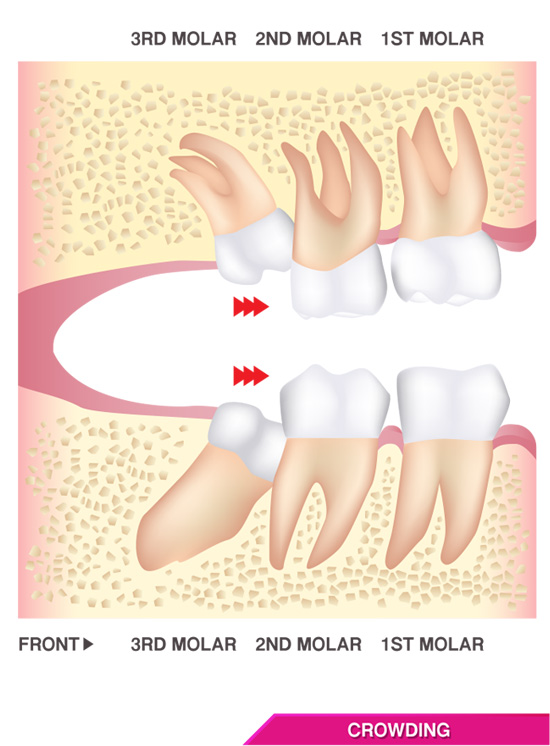
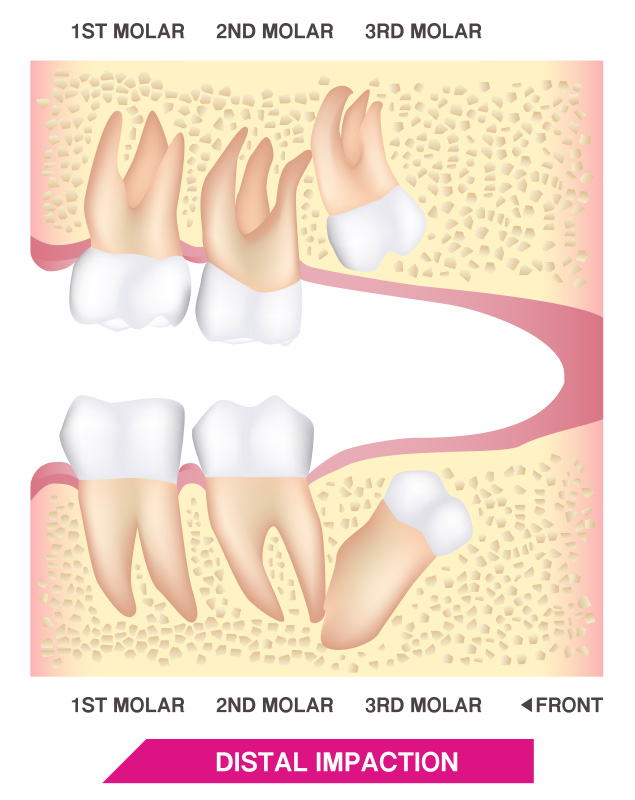
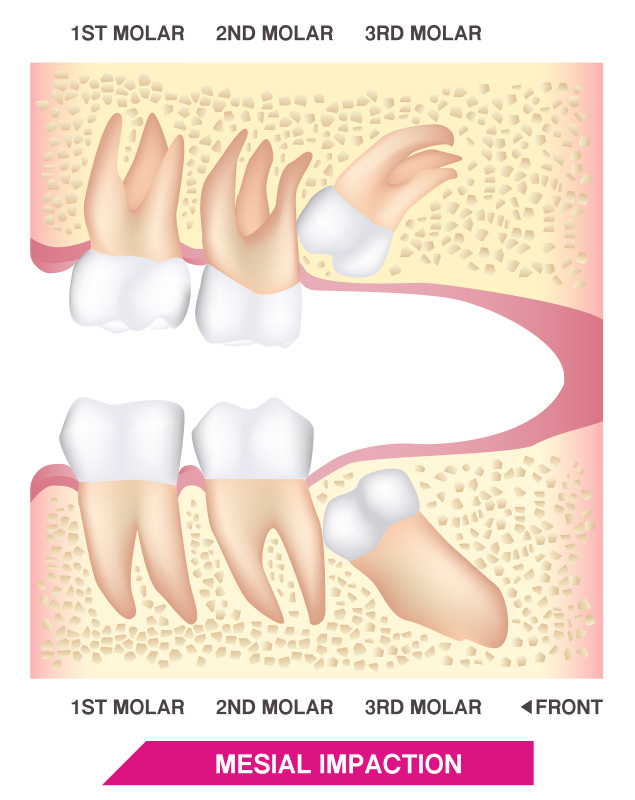
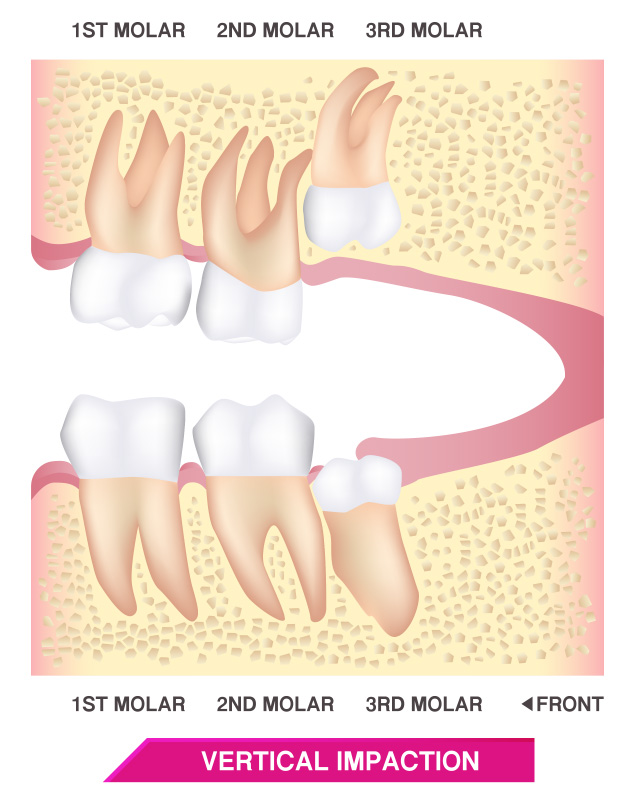
The truth is there isn't enough room in the jaw for wisdom teeth because our jaws are not large enough to accommodate the ample space required for wisdom teeth to erupt properly. Reduction in the weight of the facial skeleton is an evolutionary trend. Since there is not enough space for them to erupt properly, wisdom teeth often appear in various angles like the description shown above. This can result in toothache or jaw pain, infections leading to trismus (limited mouth opening) and halitosis (bad mouth odor), cysts, and erosion or erosive gum lesion in the oral cavity. Also, the lack of space could potentially contribute to crowding of the remaining teeth and referred TMJ pain, headache, and earache.
Third molars, commonly referred to as wisdom teeth, often damage the adjacent teeth, called second molars. Dentists and oral surgeons routinely recommend removing wisdom teeth before they cause damage or harm to adjacent dentition and anatomical structures as well as patients' overall health.
In general, as practitioners we consider the involvement of three Ps when asked "To Remove or Not To Remove" third molars:
- Pain
- Pathology (a disease process caused by the impacted third molar)
- Periodontium (meaning that the presence of a third molar is negatively affecting the gum and bone level of the adjacent second molar)
Most likely, yes.
Here is a simple exercise.
Locate a mirror and look at the back teeth at the back of your mouth; these are referred to as molars. By around the age of 12 or 13, you should see two "molars" in place. Now, think of "third molars," which are your wisdom teeth.
To see if you have ample room for your wisdom teeth, put your finger behind either second molar. If you feel a flat platform of gum tissue, there is a chance you have enough room for your third molars. If you feel the gum tissue curving upwards, then this is a sign that you don't have nearly enough room for your wisdom teeth.
This illustration is only an estimate to check for room in your mouth. There are a lot more criteria that an oral surgeon considers during the consultation. This is just a quick test to provide you with an idea of what an oral surgeon is going to do to measure the space at the back of your mouth.
Please keep in mind that appropriate clinical examination and specialized imaging are necessary to confirm a definitive diagnosis and propose a treatment plan.
- What will happen if I leave my wisdom teeth intact as they are now?
- Do I need to have all my wisdom teeth removed?
- What are the risks of surgery based on my health concerns?
- What are common complications that could arise if the procedure is not handled appropriately?
- How do my wisdom teeth rank in terms of difficulty level that you've seen?
- What are my options for anesthesia?
- Will I need to have someone drive me home following surgery?
- When can I expect to return to school or work?
- What type of diet should I be expecting after the procedure?
- When can I resume routine versus strenuous physical activity?
The ideal time to get your wisdom teeth removed is before the root is fully formed.
The wisdom teeth removal procedure becomes more complicated as patients age, roots fully develop, and jaw bone becomes denser.
Teeth grow from the crown down to the root, so if you get your wisdom teeth removed before the root develops, then the surgery is much easier, complication rates are much lower, and the recovery time is much less as well.
Keep in mind sometimes you won't be able to see the crowns or third molars due to being impacted or, in other words, being entirely covered by bone and/or gum. Therefore, if you're a teenager or young adult and are unaware of the presence of wisdom teeth in your mouth, you need to schedule a consultation with Dr. Senehi to discuss the presence or absence of third molars, and it's clinical consequences in relation to your mouth and overall health.
Wisdom teeth symptoms
The result of having too little real estate for all of our teeth is dental havoc. Due to the lack of space, wisdom teeth will often collide with adjacent teeth as they grow out in a troublesome process known as impaction.
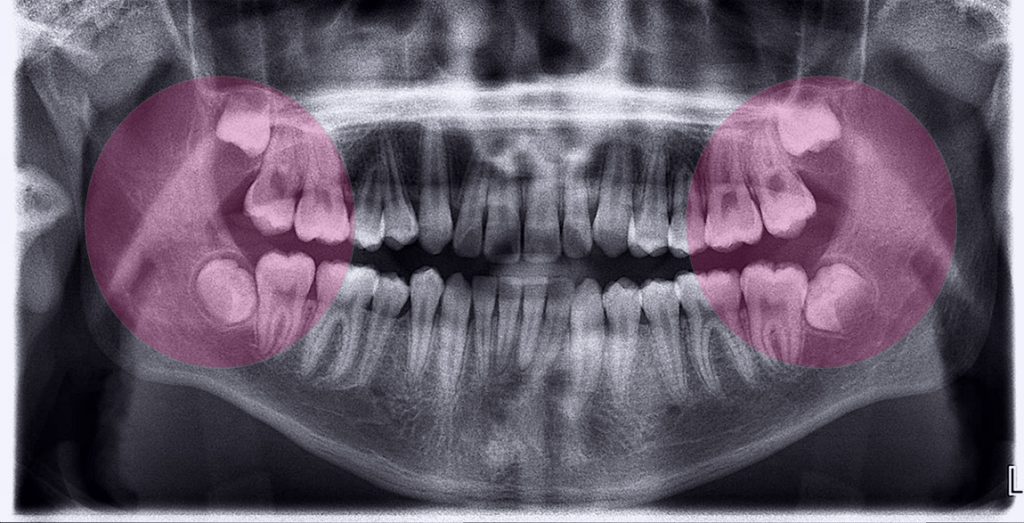
There are three broad classifications of impacted wisdom teeth:
- Soft tissue impaction
- Partial bony impaction
- Complete bony impaction
During the first, the crown of the tooth has penetrated through the bone, but still covered by the gums.
In the case of partial bony impaction, part of the tooth remains submerged in the jawbone.
Finally, during complete bony impaction, the wisdom tooth in question remains entirely encased in the jawbone.
In all three cases, impaction can result in dental crowding, localized pain and swelling known as pericoronitis, bleeding, and periodontitis. Other problems associated with wisdom teeth include partial eruptions in which a third molar only partially emerges resulting in a flap of tissue that can become a hotbed for food debris, bacteria, and potentially, the site of severe infections. In rare cases, cysts and tumors can also form as a result of wisdom teeth emergence.
Conventional wisdom in question
Despite universal agreement that removal is the best course of action for impacted wisdom teeth, there is less consensus about what to do with wisdom teeth that are not impacted or partially erupted. Research suggests that only 12 percent of impacted teeth result in any pathology. To put that in perspective, the appendix, another seemingly useless vestigial body part, has an incidence rate of pathology at 10 percent. Yet, most people don’t submit themselves to inherently risky medical procedures to have it preemptively removed. Surgery can itself have unintended negative consequences including infection, bleeding, numbness, and in extremely rare cases, paresthesia due to nerve damage. As a result, there are some in the medical community who suggest that the same caution doctors and patients apply to an appendectomy should apply to the practice of removing wisdom teeth. It is important to remember, however, that it is wise to have a consultation to determine whether or not they should be removed. Ultimately it is a judgment call by both the dentist and patient to determine the benefits or impact of removal.
Wisdom Teeth Pain
Wisdom teeth pain is, obviously, unpleasant. We will go out of our way to avoid pain if possible. That only makes sense; our nervous system evolved a pain response to warn us that something is dangerous or harmful. When dental pain or wisdom teeth pain occurs, that means something has gone very wrong in the mouth. While our bodies are great at detecting pain and directing our attention to the site of that pain, it isn’t as good at telling us what the cause is.
Dental pain, or odontogenic pain, could indicate anything from an advanced subgingival infection to a cracked tooth, or, quite commonly, dental pain could mean it’s time to get your wisdom teeth removed.
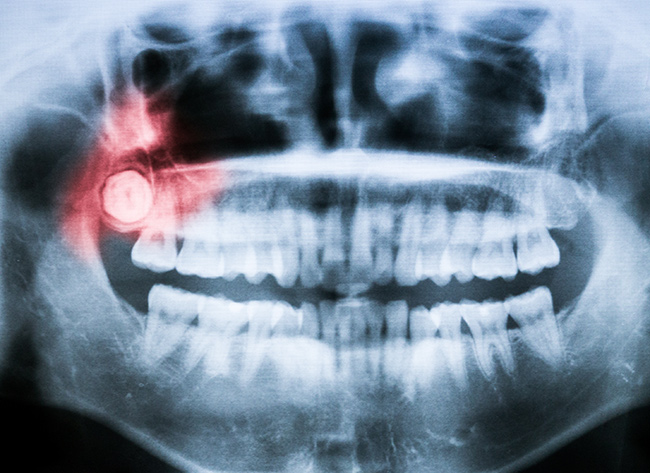
Wisdom Teeth Pain: Could It Be Wisdom Teeth Impaction?
One common underlying and often hidden cause of dental, oral, or facial pain is wisdom tooth impaction. This occurs when the third molars, more commonly referred to as wisdom teeth, become embedded in the jawbone and do not erupt as regular teeth do. This condition is commonplace and could be an explanation for your otherwise unexplainable dental or oral pain.
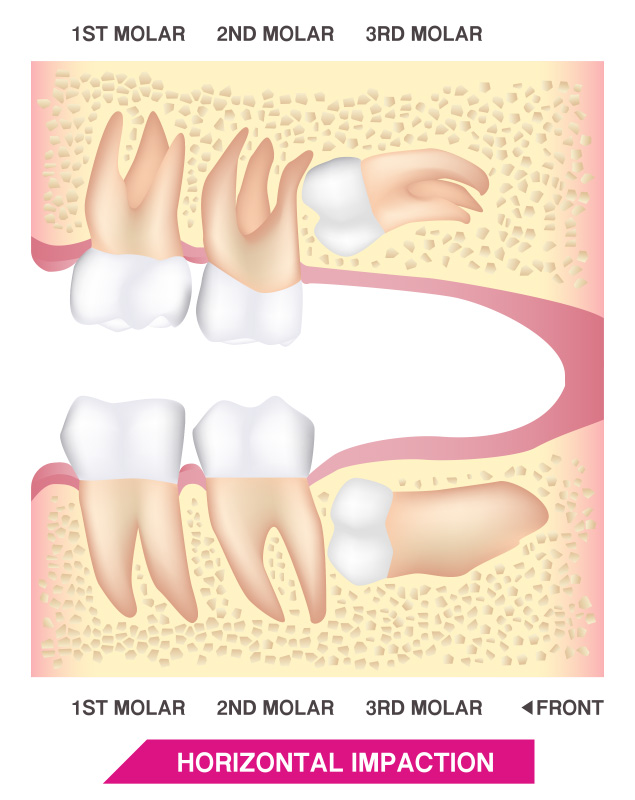
Impacted and unerupted, partially erupted, or otherwise improperly erupted wisdom teeth can cause dental and oral pain in many different ways. First, impacted third molars can actually grow against adjacent teeth, namely the second molar, resulting in dental crowding, root absorption, increased risk of infections, and as a result, wisdom teeth pain.
Wisdom Teeth Impaction
Misdirected wisdom teeth can also grow in perpendicular to other teeth or sometimes even angle back into the jaw as well as cause gums to swell and bleed. In rare cases, wisdom teeth can put pressure on the nearby inferior alveolar nerve causing pain and even headaches. Painful cysts and tumors can also develop around the area of an impacted wisdom tooth.
Pain engendered by an impacted wisdom tooth, however, is not always obvious. Two-thirds of dental patients with impacted wisdom teeth actually report no pain at all, while others may only indicate a vague pain that may or may not be centered around the impacted wisdom tooth. As mentioned above, misdirected wisdom teeth can even be the root cause of headaches and pain in other areas of the face and mouth.
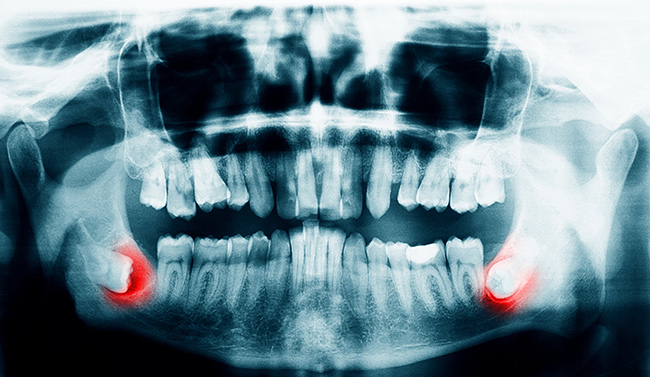
Wisdom Teeth Impaction
In a normal healthy jaw, adult teeth grow up and out of the jaw and into the mouth in a process known as dental eruption. Everyone experiences tooth eruption at some point and this natural process plays an important role in the development of children into adults, both physically and socially.
The third molars, also known as wisdom teeth, are the very last set of teeth to erupt and are thus, often imbued with a sense of social and emotional weight. Many consider wisdom teeth eruption to be a coming-of-age of sorts.
Unfortunately, because the third molars are the last teeth to erupt they are also the cause of many dental problems and concerns. Often times there is simply not enough space in the jaw to accommodate the third molars, resulting in impaction. As a result, there is a high likelihood of experiencing impaction.
Dental impaction as a result of misdirected third molars is quite common. 44 percent of patients between the ages of 25-29 years of age who opted to retain their third molars experienced some sort of impaction, either partial or complete.
Wisdom Teeth Impaction: Signs & Symptoms
There are several degrees of impaction depending on the angle and direction of the eruption of the impacted tooth. Depth compared to the biting surface of adjacent teeth, and the amount of the impacted tooth’s crown that either extends through the gums or remains within the bone also indicate degrees of impaction.
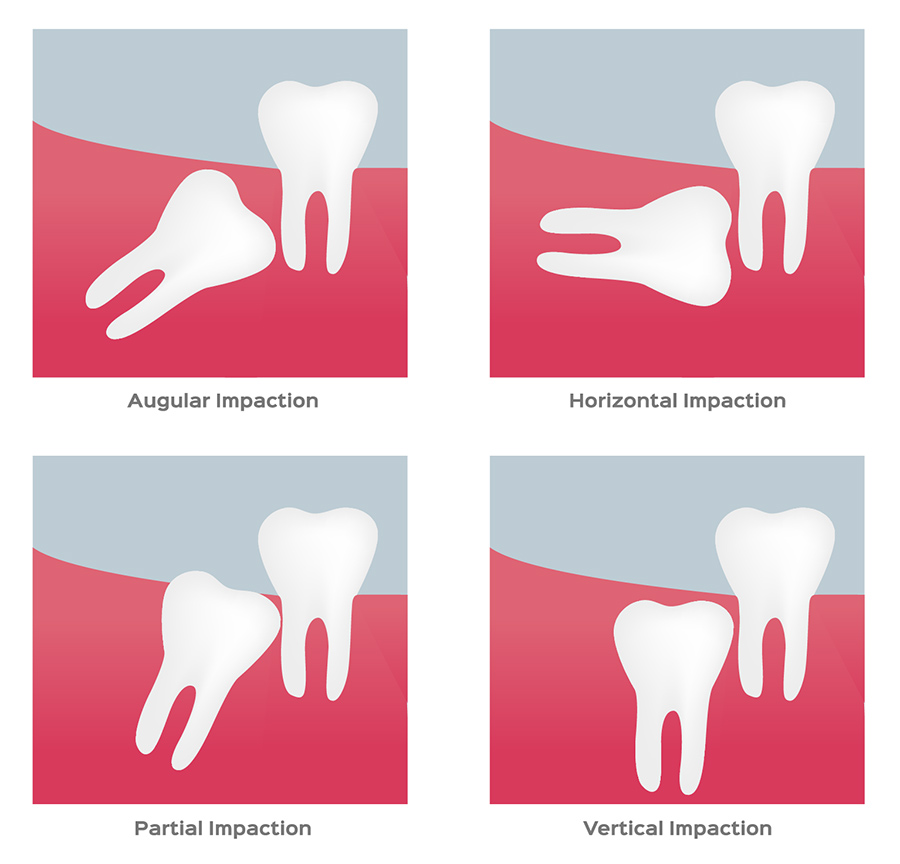
These, in turn, can result in different symptoms and dental concerns. For example, soft tissue impaction involves wisdom teeth that have grown out of the jaw bone but are still totally or partially covered by the gums. A partial bony impaction occurs when a tooth has only partially emerged while the rest of it remains embedded in the jaw bone.
Finally, a complete impaction is when the tooth is completely encased in bone. Each individual patient may experience any of these types of impactions, all of them, or none at all. Some patients may not initially experience symptoms until much later in life while a few will never have any issues with their wisdom teeth.
One of the most common symptoms of an impacted tooth is pain or a sense of pressure in the back of the mouth. This can occur for a number of reasons including pressure on the nerves of the jaw as well as infections.
Other common symptoms include tender, red, swollen, or bleeding gums, as well as jaw pain, bad breath, and difficulty opening and closing your mouth. Less common symptoms include swelling in the neck and shoulders and unexplained headaches.
Wisdom Teeth Impaction: To Treat or Not To Treat?
The standard treatment for wisdom teeth impaction is extraction. Only by completely removing the offending wisdom tooth can symptoms be alleviated. Many oral surgeons, dentists, and dental professionals recommend preemptive or prophylactic extraction of impacted wisdom teeth before symptoms arise. This common "wisdom" has given rise to the tradition of extracting wisdom teeth from young adults in their late teens.
In recent times, the wisdom of removing wisdom teeth has come under questioning. Dental extraction is still surgery and carries with it some risks, though minor. The best way to make an informed determination about whether to undergo a wisdom teeth removal procedure or retain an asymptomatic third molar is to consult with your dentist or an oral surgeon like myself.
When should I consider wisdom teeth removal?
Generally speaking, if the wisdom teeth are impacted or otherwise causing pain and distress, they should be removed. Many doctors, dentists, and dental professionals recommend removing wisdom teeth even before impaction occurs or other issues arise. For many in the field, it is far better to remove them before they cause problems. Most individuals who choose to have their wisdom teeth preemptively removed have their third molars extracted between the ages of 16 and 25, to minimize complications during surgery and have a smooth recovery. Ultimately, whether or not to extract and remove one, two, or even all of a patient’s wisdom teeth will have to be a conversation between a patient and their dentist. At the end of the day, it’s a judgment call.
Wisdom teeth removal cost
The costs of removing wisdom teeth will vary from patient to patient, from one office to another, and across geographical locations. What each patient pays out of pocket will also vary depending on what insurance, or lack thereof, he or she has. One strategy many patients pursue is to opt to have all their wisdom teeth, even those that aren’t causing any issues at the moment, removed in one session in order to pay for the administration of local anesthetics only once. Broadly speaking, extraction costs can vary depending on the complexity of the job and many other factors.
What To Expect
Wisdom teeth removal is a standard procedure millions of Americans opt to undergo every year. For many patients, wisdom teeth removal has come to signify a coming of age and a rite of passage into adulthood. Indeed, wisdom teeth, also known as third molars, are the last set of teeth that leave the mouth. Unlike baby teeth, however, wisdom teeth won’t come out naturally. Instead, they must be removed with skill and precision. Also unlike baby teeth, wisdom teeth removal is significantly more involved.
Here’s what you can expect.
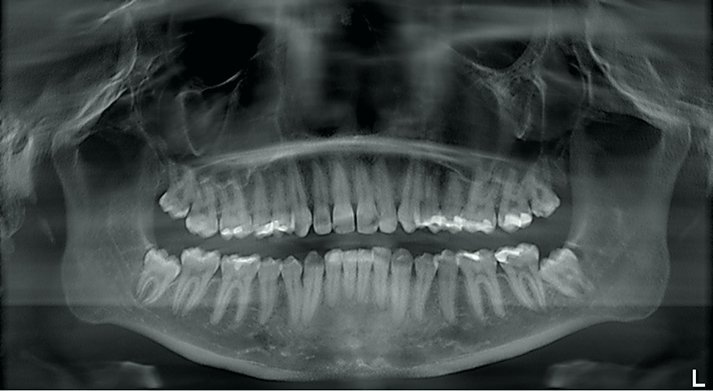
Preparation for Wisdom Teeth Removal
The first step to wisdom teeth removal is preparation. This means as a dual degree, DDS. MD. Oral & Maxillofacial Surgeon, I conduct a thorough and rigorous evaluation of the patient’s existing oral and physical health including taking x-rays to assess the position, condition, and accessibility of the wisdom teeth in question.
Once the images and other diagnostic data have been assessed, I will provide the patient my advice about how to best address wisdom teeth removal. A treatment plan is developed, with input from the patient, that prioritizes a very smooth process with minimal impact to the mouth and jaw as possible.
Patients will also be asked about any allergies, in particular, allergies to different categories of medications or dental anesthetics and sedatives that could potentially cause unnecessary complications. Another important factor I take into consideration is a patient’s prescription medicine use. Managing patient's routine prescription regimen significantly influences the preparation process. Once everything has been reviewed, an appointment is set for the procedure, and the patient receives an email containing a checklist in preparation for their appointment at Facial & Oral Surgery Institute.
On the day of the surgical procedure, we ensure the following precautions have been enforced. First, we make sure patients have someone they trust who will drive them home after the procedure due to the lingering effects of anesthesia. Depending on the type of anesthetics used, specific restrictions previously explained in detail will be confirmed making sure patients are compliant with guidelines which affect the safety and efficacy of the procedure.
The Wisdom Teeth Extraction Procedure
The wisdom teeth procedure begins with anesthesia, either local anesthesia, or intravenous sedation which itself divides into three different categories, light, moderate, and deep, or in rare cases general anesthesia.
Local Anesthesia
Local anesthesia only numbs the surgical site. In effect, patients will remain awake and aware of the procedure. However, they will not feel any pain. Patients also feel the mechanical pressure involved during the removal process.
Intravenous Sedation (Light. Moderate, Deep)
Sedation anesthesia, "Twilight Zone" works a little differently. Sedation anesthesia is typically administered via intravenous (I.V.) drip and lowers the patient’s consciousness to a very relaxed state of mind. Most patients will have no memory of the procedure and will feel no pain.
General Anesthesia
A small percentage of patients will receive general anesthesia. With general anesthesia, the patient is rendered entirely unconscious.
Anesthesia is necessary not only for patient comfort but to also ensure that the patient does not move or flinch during the procedure which can disrupt the delicate extraction process. Also, it helps patients to keep their mouth open for a relatively long period of time with no difficulty.
Once a patient is appropriately anesthetized or sedated, the wisdom tooth extraction procedure begins. Unlike extraction of other teeth, wisdom teeth extraction is unique in a sense where it requires a skilled surgeon, typically an oral & maxillofacial surgeon, such as myself who can perform the operation.
The surgeon will begin by making an incision into the gum and soft tissue in order to expose the bone and tooth. Incision design significantly influences the rate of damage to surrounding neurovascular structures, resulting in irreversible complications, as well as reducing the time it takes for the site to close. Some bone around and adjacent to the wisdom tooth may also be removed to facilitate the removal process.
For wisdom teeth that are severely impacted, additional bone may need to be removed in order to minimize complications during removal. Often, a wisdom tooth will be removed in sections in a process known as controlled tooth division. This is accomplished with special tools which divide the tooth into more manageable pieces for removal. When ready, either extraction forceps or a dental elevator is used to extract the tooth.
With the tooth removed, there is still plenty to do. It is critically important for my surgical team to assist me in cleaning the surgical area of any debris and remaining tooth remnants. When the extraction site has been thoroughly cleaned, stitches or sutures may be used to close the wound. A gauze pad is placed over the extraction site to stop the bleeding and to help a blood clot form that will naturally close the site and allow it to heal.
Post-Operative Care and Considerations
Post-extraction bleeding and discomfort are common but hopefully minimal. Bleeding can occur within 24 hours after the operation. If sustained, heavy bleeding occurs with no signs of lessening, patients should contact my office for immediate assistance.
To lessen bleeding, patients should place a piece of clean gauze over the site of extraction and apply steady pressure by biting down for thirty minutes to an hour. The key is to use pressure over an extended period of time to help the body form a natural blood clot. In cases where bleeding is anticipated, I will often utilize a clotting aid during the procedure such as absorbable collagen or gel-based dental dressing. The process of wisdom tooth extraction is very critical and it will require a trained surgeon with extensive experience to deal with intraoperative complications and manage them appropriately.
To minimize bleeding and avoid dislodging a blood clot, patients should refrain from rigorous rinsing or spitting, strenuous exercise, hot food, carbonated beverages, sucking through a straw, smoking, or touching the extraction site with their fingers or tongues.

Wisdom Teeth Procedure Recovery
Once the initial 24 hours has passed, taking care of a wisdom tooth extraction site is much more comfortable. Patients are generally advised to avoid doing anything that will irritate or damage the extraction site. In general, patients should keep the surgical site clean and avoid activities, such as contact sports, that might traumatize the site and disturb the healing process. At Facial & Oral Surgery Institute, we're constantly in the process of educating our patients regarding the pre and post-operative instructions in an attempt to prevent complications. Following post-operative instructions significantly improves the outcome of the procedure.
Eating habits
Eating habits will also have to be temporarily altered. Patients should be careful not to chew food directly on or near the wound. Patients will generally be on a soft diet for a minimum of two weeks after the procedure.
Socket Irrigation
After a few days, patients will need to start irrigating their extraction sockets to remove debris and prevent infections. Socket irrigation is accomplished by a syringe with a curved tip and filled with either salt water or prescribed antibiotic rinse. Typically, the irrigation process only lasts as long as it takes for the wound to completely close.
Controlling pain, discomfort, and swelling
Most symptoms after a wisdom tooth extraction will typically go away 24 to 72 hours after the initial surgery. Pain, discomfort, and swelling can be controlled with prescribed and over-the-counter pain and anti-inflammatory medication.
Most Popular Questions Regarding Socket Irrigation
- Rest - Immediately following wisdom teeth extraction you should rest and allow the effects of anesthesia to wear off and for a blood clot to form and protect the wound. The gauze provided by your oral surgeon is intended to put pressure on the wound area, promote blood clotting in the extraction socket, and to help reduce bleeding. Your oral surgeon will provide instructions on how to change the gauze as needed.
- Avoid eating for at least 2 to 3 hours.
- Avoid alcohol, coffee, soft drinks, or any drinks containing sugar. Also, do not use a straw to consume beverages for at least the first several days.
- I do recommend any cooled down food or frozen beverages such as popsicles, ice cream, yogurt, or thin soup that doesn't promote the temptation to chew.
- Take painkillers such as ibuprofen as needed but avoid aspirin or any substitute that contains acetylsalicylic acid (ASA) which can cause prolonged bleeding in the extraction site area.
- Use ice or gel packs to reduce swelling and pain if needed. The "newer" soft or gel ice packs are easier than the traditional ice packs that use actual ice. The "newer" packs last longer and provide better contact and conform to your jaw area much easier.
Keep in mind that the extraction socket area may bleed for a few days. See your oral surgeon if bleeding is continual or heavy and doesn't stop.
Dry Sockets
While having dry sockets may not sound alarming, having dry sockets after a wisdom teeth extraction procedure can result in extreme pain for the patient. Dry sockets, or alveolar osteitis, can sometimes occur after a wisdom tooth extraction or tooth removal procedure. While doctors aren’t exactly sure why some patients experience the condition while others do not, it is theorized that dry sockets result when the initial post-extraction blood clot either fails to form, dissolves too soon, or is somehow otherwise dislodged.
Typically, the initial clot develops a protective layer over exposed nerve endings and exposed bone and provides a structure for new bone to grow and for the healing process to begin. When the clot is dislodged or destroyed, underlying nerves and bones can become exposed to food debris and bacteria leading to painful, recurring infections that can delay healing and even permanently damage the jaw bone.
What is the rate of incidence for dry socket?
Dry Sockets: Signs & Symptoms
The most noticeable sign of dry sockets is severe pain in or around the extraction site a few days after the initial operation. This is a sign that the blood clot has become dislodged, exposing raw nerve ends and underlying bone to the elements. This can be visually confirmed by looking at the extraction site and seeing an empty or “dry” socket. In many cases, the underlying bone itself may even be visible. Other signs include radiating pain extending from the site of the surgery to the eye, neck, or ear on the same side of the face. When a socket becomes infected, a foul odor can also emanate from the back of the mouth as well as produce an unpleasant taste or odor.
The best way to avoid the potential complications associated with dry sockets after wisdom teeth removal is to seek an oral surgeon with extensive tooth extraction experience. A skilled oral surgeon can perform a clean extraction, leaving no dental debris behind that could compromise the extraction site. Furthermore, he will also minimize the surgical impact and trauma on the extraction area, perform a thorough cleaning of the site of the surgery, and if necessary, suture wounds cleanly.
Most Popular Questions Regarding Dry Sockets
Yes, a dry socket can occur even if you have stitches. A dry socket is an unfortunate situation that can develop following tooth extraction. Dry sockets tend to occur after 4 to 6 days in the healing process following tooth extraction. What happens is the blood clot that is formed in the cavity that was previously occupied by your tooth becomes dislodged, exposing the bone underneath. It is not an infection, and the good news is the extraction site will continue to heal normally, but it does prolong the healing time of the socket. Typically the pain becomes very severe and unbearable.
If you are a patient of Facial & Oral Surgery Institute, we recommend you immediately contact our office.
Dry socket prevention isn't very complicated, as long as you care for the extraction site properly. Following are some tips on how to keep the extraction site clean and healthy during the recovery process:
- Food and Beverages: Following your wisdom teeth removal you likely won’t feel like eating, but that soon passes and you begin getting hungry. I highly recommend you stick to soft foods and carefully chew on the opposite side of the extraction site if possible. Also, stay hydrated and drink plenty of water. Avoid soft drinks with sugar or caffeine as well as alcoholic beverages. Do not use straws for at least 7 to 10 days or for as long as your oral surgeon recommends. The suction could cause undue pressure and dislodge the blood clot.
- Tobacco: The most common cause of dry socket is from the use of tobacco. Avoid it! The Mayo Clinic published a warning that smoking or chewing tobacco within 48 hours of surgery slows the healing process and patients can have painful repercussions. Also, smoking introduces bacteria into the surgical area of the extraction and disrupts the healing clot.
- Rest: It is ideal to get off your feet and rest and allow some time for the effects of the anesthesia to wear off and for the healing process to occur around the surgical area of the tooth extraction. Avoid sports or strenuous activities that can disrupt the blood clot and healing process. If you are experiencing pain take ibuprofen or acetaminophen and contact your oral surgeon if the pain worsens, radiates through your face, or is accompanied by swelling, redness, and/or fever. Avoid painkillers containing acetylsalicylic acid (ASA), such as aspirin, as they can cause prolonged bleeding.
- Dental Hygiene: Follow the directions of your oral surgeon on replacing gauze or cleaning the extraction area. It is best to wait for 24-hours before you clean the extraction area. You can very gently brush your other teeth and your tongue after the first day. You may also gently rinse with an antibacterial mouthwash such as Colgate Total® Advanced Pro-Shield™ Mouthwash to remove germs that could infect the area of your tooth extraction.
A wisdom tooth extraction can be unsettling, but as long as you follow your oral surgeon's instructions, your recovery should be uneventful. Dry socket can disrupt your healing process, so make sure that you're conscious of your eating, drinking and hygiene habits in the days following your extraction, to have the best chance of avoiding the issue altogether.
Dry sockets are a glitch in the healing process. Dry sockets don’t prevent recovery or cause significant problems, except for the excruciating pain that having one creates. So yes, they should heal on their own.
However, getting treatment from your oral surgeon will do two things:
- Your oral surgeon will ensure no infection occurs. Usually, an antibiotic is prescribed.
- Your oral surgeon will make sure to provide a prescription to deal with the pain.
Also remember, dry sockets are pretty rare, and even more so on upper extractions. The most common spot is a lower molar extraction, and still, it’s less than a 3 percent chance a patient will experience a dry socket. If you’re not sure if you have a dry socket, you likely don’t. The level of pain is fairly intense because the bone beneath your extraction is exposed. This is something you will know if you have it. The pain is not subtle at all.
To manage to prevent a dry socket I recommend you avoid the following situations for 3 to 4 days after your wisdom tooth extraction:
- Exercise
- Drinking soft drinks, alcohol, or sparkling water.
- Drinking from a straw
- Smoking
- Coughing or sneezing
- Brushing where the tooth was extracted
Dry socket pain is almost unbearable. Post-extraction pain peaks and wanes within a 24-hour period, but dry socket pain peaks three to five days after the wisdom tooth removal and can often take weeks to go away unless treated by an oral surgeon.
The most common symptoms include bad breath, headache, earache, and a foul taste in your mouth.
Oral surgeons will pack the socket with materials to insulate the bone. This will alleviate the pain during the extended healing process as well as mimic what the blood clot would have achieved.
Two-Ways An Oral Surgeon Can Pack the Dry Socket:
- Packing the surgical area of the socket with a special paste that will promote healing and alleviate the pain almost immediately. This method relieves the pain right away but is considered to be a short-term solution.
- Pack the surgical area of the socket with bone graft material or surgical foam. This is considered a long-term solution but it is also more expensive.
There are several considerations when it comes to antibiotics. However, a good rule of thumb is whenever there is pus present in the mouth, it is wise to consider antibiotics.