Contents
Chapter 6
Types of Oral and Dental Diseases
Chapter 7
Treating Oral and Dental Problems
Chapter 8
Surgery for Oral and Dental Problems
Chapter 9
What Can Go Wrong?
Chapter 10
Keeping Your Teeth and Gums Healthy
Chapter 11
What Men Need to Know About Oral Health
Chapter 12
What Women Need to Know About Oral Health
Chapter 13
What People with Diabetes Need to Know About Oral Health
Chapter 1
Maintaining Excellent Oral & Dental Health

The Big Three
Good oral health plays a crucial role in a person’s overall health and self-esteem. That’s why it’s important for everyone, children and adults alike, to invest the time, energy, and resources into protecting the health of their mouth.
Fortunately, with the right habits and dental hygiene practices, enhancing and maintaining good oral health is as easy as 1-2-3.
Following are the three cornerstones of a healthy mouth that everyone should strive to incorporate into their oral health routines.
Brushing your teeth is the foundation of every effective dental and oral health routine. Brushing promotes oral health on several fronts. First, by removing food debris and leftover scraps, brushing eliminates a potential fuel source for destructive bacteria. Secondly, by scrubbing away plaque and bacterial biofilm, brushing physically removes the bacteria and makes it harder for new microbes to establish a foothold. Finally, when combined with fluoridated toothpaste, twice-per-day brushing aids in the remineralization of dental enamel.
The Bottom Line: Brush every day, twice per day for a few minutes with a fluoridated toothpaste.
Only 40 percent of people floss once per day as recommended by dentists and oral health professionals. While often overlooked or misused, flossing plays a crucial role in a person’s dental health, but should be incorporated into everyone’s oral health regimens. Flossing, like brushing, relies heavily on mechanical action to physically remove plaque, food debris, and other accumulation of biomatter that can lead to the proliferation of bad bacteria. Flossing is particularly useful for cleaning in between the teeth and other spots in the mouth that brushing often misses.
The Bottom Line: Floss at least once a day and especially after meals.
No one cleans teeth like a dental professional, typically a hygienist can clean teeth. Furthermore, many of the specialized tools and equipment, such as a dental scaler, simply aren’t found in most homes. A professional cleaning also referred to as a dental checkup, is more than simply a dental cleaning. Visiting a dental clinic in person gives the hygienist and supervising dentist an opportunity to assess your oral health. They can catch any potential oral health issues early, including signs of dental caries or even oral cancer, and make the appropriate recommendations.
The Bottom Line: Visit a dentist every 6 months minimum for a dental checkup.
5 Steps to Maintaining Excellent Oral Health
Brush your teeth twice a day.
Brush with a fluoridated toothpaste.
Floss at least once a day, especially after meals.
Check your gums and mouth regularly for signs of injuries or infections.
Visit a dental clinic every six months to a year for regular checkups.
Chapter 2
Facts About Oral & Dental Health
"The more you know and are aware about oral and dental health, the better you’ll be able to make good oral and dental health decisions."
NAVID SENEHI, DDS. MD.
Diplomate of American Board of Oral & Maxillofacial Surgery
Chapter 3
15 Common Oral Health Myths (and Why They're Wrong)
The public discourse on dental and oral health is, unfortunately, often rife with misinformation and downright wrong opinions that may cause some to make poor oral health decisions. Check out these 15 common oral health myths so you can stay informed and make the right decisions based on factual information.
False. Only a tiny fraction of a patient’s oral microbiome negatively affect oral health. The rest compete with these so-called “bad bacteria” and should be cultivated in order to out-compete harmful microbes.
False. While the toothbrush mechanically removes plaque and debris, toothpaste introduces fluoride which is important for the remineralization of teeth.
False. Flouride in the safe dosages found in many well-maintained municipal water supplies and in toothpaste is safe and incredibly important for oral health. Water fluoridation is often described as one of the most important oral health advancements of the 20th century.
False. Bacteria, and the acid they produce as a by-product proliferates rapidly. Once destructive bacteria is allowed a foothold, it can cause damage to the enamel in a matter of hours.
False. Flossing physically remove food debris and buildup from in between the teeth where brushing may not be as effective. It is very important to any dental health routine.
False. Dental checkups allow dentists to not only thoroughly clean your teeth but also catch any potential oral health issues before they get out of hand. An ounce of prevention is worth a pound of cure.
False. Professional cleanings can only be performed by a trained hygienist or a dentist. Not only do they possess the commercial-grade tools necessary for a thorough dental cleaning, but they also know how to use them safely and effectively. Dental professionals, such as hygienists and supervising dentists, are also able to identify oral health problems quickly and deal with them on the spot or recommend an appropriate solution.
False. Dental or oral surgery should be performed by an oral surgeon who is both qualified and experienced in such matters. Just as you wouldn’t want a family doctor to perform brain surgery, so too you would not want a general dentist to perform oral surgery.
False. While sugary foods are bad for your teeth, simple carbohydrates are equally as bad for your teeth. Carbohydrates behave like sugar in the mouth and help fuel harmful bacteria.
False. Dental health is critically tied to the rest of the body. For example, periodontal disease increases the risk of heart failure.
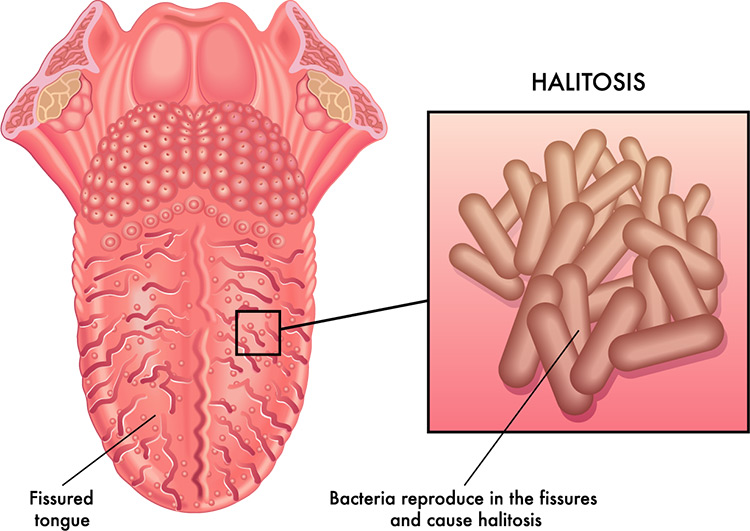
False. Bad breath, or halitosis, can be the result of a variety of factors that are both oral or completely unrelated. While halitosis is a sign of periodontal disease, it is also a sign of cavities, hidden abscesses, oral cancer, and a number of other oral issues. In addition, bad breath can also be the result of simple genetics or a diet high in animal protein and fats. To address bad breath, see a dentist to help identify the underlying cause.
False. Bloody or sensitive gums are a sign of gum disease or periodontal disease and should be taken seriously.
False. Pain is often a sign that things have already gone awry. However, many oral diseases, such as early-stage periodontal disease or a cavity that hasn’t penetrated the dentin may not exhibit noticeable pain. To prevent pain before it happens, visit a dentist regularly for routine dental and oral health checkups.
False. Brushing harder will actually result in toothbrush abrasion and subsequent gum recession.
False. While incredibly resilient considering the amount of physical stress and abuse we put out teeth through, they are also very vulnerable to disease and decay. That’s why dental and oral health is so important. A good dental and oral hygiene routine, coupled with preventative measures, will go a long ways towards preserving your natural teeth well into old age.
Chapter 4
Top 10 Signs & Symptoms of Oral and Dental Disease
It is important to recognize the signs of oral or dental disease.
Early diagnosis and treatment are key to curing early-stages of oral and dental diseases and for reversing any damage that may have already occurred.
Signs and symptoms of oral or dental disease may not always so obvious or associated with pain. Nor do oral diseases always show obvious outward symptoms. For example, chronic periodontitis, may not become obvious until after a catastrophic infection or tooth loss. Many oral diseases are progressive in nature and begin with minimal signs or symptoms and therefore are often dismissed as an annoyance rather than a problem.
As an Oral & Maxillofacial Surgeon, I am often confronted with the results of years of dismissing viable signs and symptoms as a result of dental disease. Often I see patients who are past the point of prevention and in some cases past the reversal of damage.
While we are more than able to perform cosmetic restorative surgery that enhances or transforms a patients teeth, sometimes the best cure is proactive prevention treatment.
Top 10 Signs of Oral and Dental Disease
Pain
Ulcers or Sores
Tooth Loss
Bleeding or Swollen Gums
Bad Breath
Sudden Sensitivity
Receding Gums
Facial Swelling
Clicking Jaws
Perpetually Dry Mouth
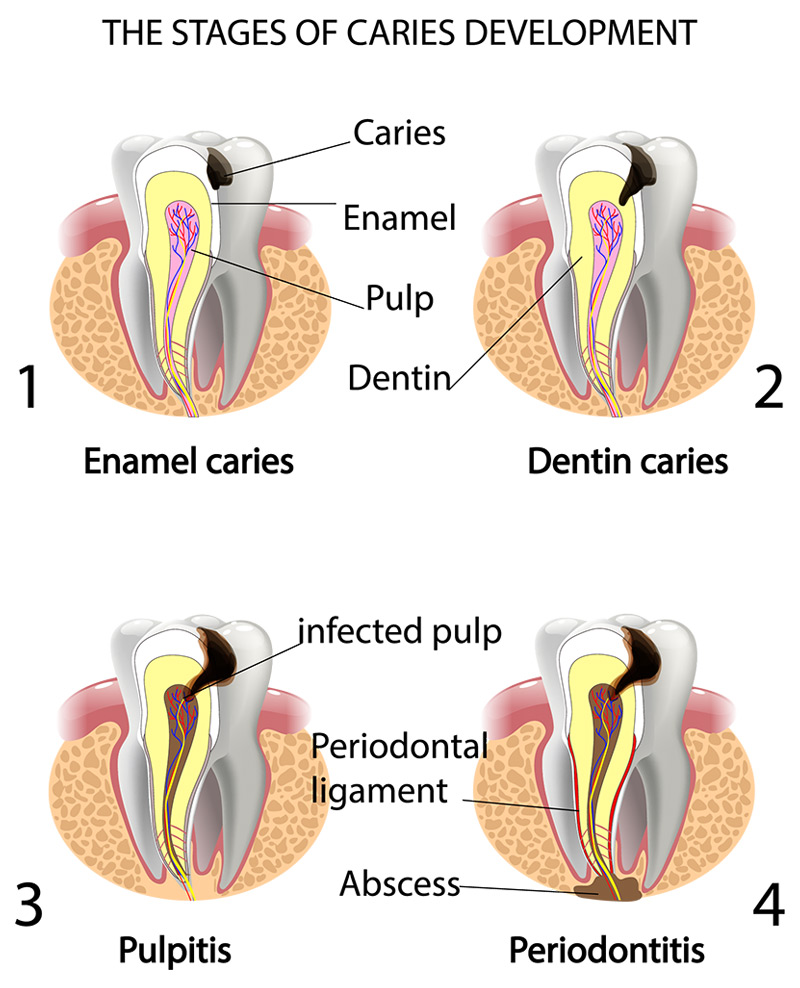
Pain is the most visible sign and an indication of an oral or dental problem. Unfortunately, by the time pain is present it can be too late.
For example, teeth pain is often the result of an infection either from ongoing damage to the dental enamel and underlying dentin which has reached the sensitive inner pulp, or it could be an infection in the underlying jaw bone. It's possible at this point that the tooth is beyond preserving and may require being extracted.
Seeing early signals and taking action could likely prevent the loss of teeth.
In any case, once you notice pain in the mouth, jaw, face, or neck you should see a dentist as soon as possible. When pain is present, it’s time to take action and not prolong the situation. Even a mild ache or dull pain can be a sign of an advanced underlying disease.
Ulcers and sores are a sure sign that something may be amiss.
Most of the time, small ulcers and sores in the mouth may be nothing more than canker sores or cold sores. This is not always the case though.
You should be especially wary of ulcers or sores that remain for long periods of time, that appear without explanation, show a change in color, or seem to grow in size. These can be signs of something much more severe, such as an infection, infectious mononucleosis, hand, foot, and mouth disease, celiac disease, an autoimmune disorder, or oral cancer.
Be prepared to monitor minor sores and ulcers, and see us immediately if you notice the ulcer spreading, growing, or refusing to go away.
Signs of serious disease include ulcers with white patches may be a sign of leukoplakia or oral lichen planus.
Unexplainable tooth loss, or loose teeth in adults, is a major problem.
Tooth loss means that either the tooth itself or the underlying jaw bone has lost structural integrity. That is not good. Tooth loss and loose teeth often point to severe dental decay or periodontal disease. Worse, if left unaddressed periodontal disease can spread throughout the jaw resulting in widespread bone destruction. In some cases, rampant periodontal infections can even be fatal.
Even if the underlying infection is contained, the damage to the bone is often permanent and irreversible. Once a tooth is lost, there is no going back. Thankfully, patients who have lost teeth as a result of natural aging, periodontal disease, or even trauma can replace their missing teeth with natural-looking, natural-feeling artificial teeth called dental implants or All-On-4 dental implants.
Bleeding, particularly during brushing and flossing, is quite common. Along with swollen gums, bleeding from brushing and flossing is a surefire sign of some form of gingivitis. These are natural physiological responses to infections in the soft tissue.
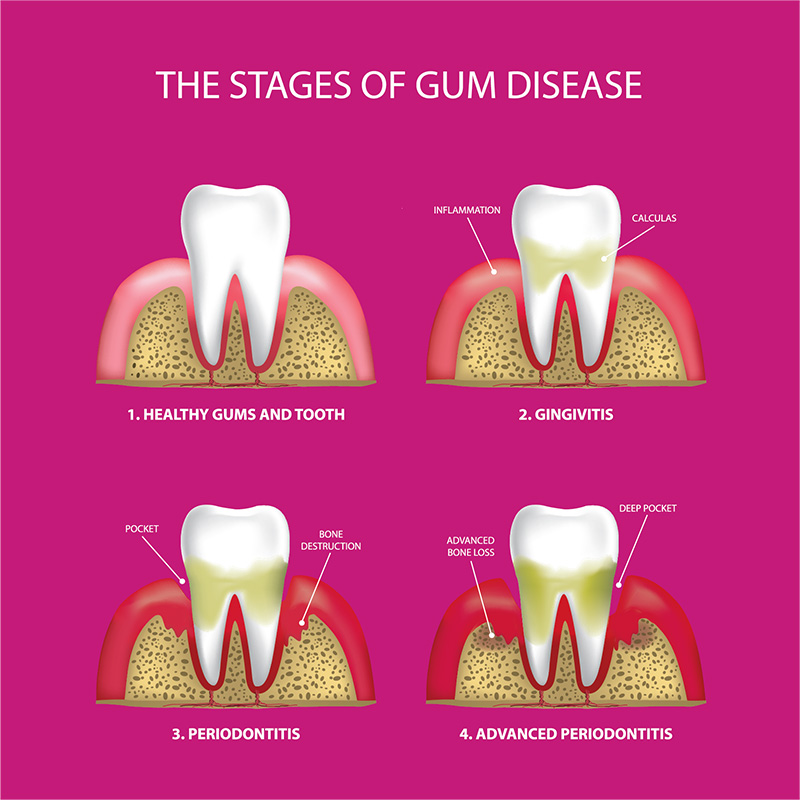
While common, bleeding and swelling in the gums should never be overlooked. Many who exhibit such symptoms of gingivitis will go on to develop a periodontal disease which can impact a person’s oral health.
The only way to reduce or eliminate bleeding, swelling and other symptoms of low-grade gingival infection is to brush and floss correctly and get regular dental checkups.
Inflamed gums that bleed with gentle probing often indicate gingivitis has progressed and periodontal disease may not be far behind.
Nothing is more embarrassing than being told that you have bad breath, often called halitosis. Halitosis isn't always cured by chewing gum or brushing your teeth. Often times bad breath is simply the result of poor oral hygiene habits. Chronic bad breath that does not respond positively from a thorough oral and dental hygiene routine can often be a sign of something else or a symptom of dental caries or periodontitis.
Also, the bad odor may be the result of tooth decay. Periodontal disease not only causes bad breath but can also be accompanied with a foul taste in your mouth as well.
Dental sensitivity is the result of worn enamel or a penetration in the tooth that has reached the sensitive dental pulp beneath the enamel.
The enamel, or hard outer shell, of a tooth, does not have nerve endings or “feel” pain or sensitivity. Any dental sensitivity, particularly to hot or cold, is a sign that the enamel may be in trouble. For those with fillings, it may indicate that the filling is worn or loose and needs to be replaced. It may also indicate that an infection is present around the edges of the filling.
Sensitive teeth and worn enamel may also be a sign of bruxism or teeth grinding.
Even when sensitivity to hot or cold is relatively mild and there is no chronic pain, I recommend you have it checked out by a dentist or oral surgeon. At the very least if a thinning enamel is a problem a dentist can recommend a treatment plan for sensitive teeth.
In the worst case scenario, the dentist may uncover a micro-cavity or infection that needs to be treated. In any case, it is far better to identify the potential problems rather than letting them become a more severe problem later.
Receding gums can be the result of either toothbrush abrasion, gingivitis, or periodontal disease.
Early detection and treatment of receding gums are critical for oral and dental health. Unlike some soft tissue injuries, gum recession can become permanent if not addressed early.
In early stage gingivitis, mild gum recession can be stopped and the damage reversed. However, once gum recession has progressed past a certain threshold, the gums become permanently detached from the teeth. Once detached, periodontal disease is inevitable.
Healthy gums form a tight bond with the teeth preventing food debris and bacteria from getting beneath the gums and reaching the dental roots. However, once gums have receded the natural seal is loosened resulting in pockets of infection. Worse, the body will not naturally heal or repair that natural seal.
People with severe gum recession must undergo regular deep dental cleanings in which the dentist must clean and scrape well below the gum line in order to remove debris and plaque.
Facial cellulitis, or swelling, is often a sign of a severe oral infection or deep dental abscesses and should be taken seriously.
Once signs of facial swelling become apparent, I recommend you see us at Facial & Oral Surgery Institute. A deep dental abscess is often the result of a cavity that has been left untreated for a prolonged period of time. When a cavity has reached this critical stage, it has long eroded the enamel, dentin, and inner pulp and becomes a threat to the jaw bone and beyond.
It is critical to take facial cellulitis, or swelling, very seriously.
Call us immediately or call 911 if the swelling spreads to the upper part of the face away from the jaw or to the neck. Swollen eyelids, unusual drowsiness, weakness, fainting, or difficulty swallowing and breathing are serious signs and symptoms of an oral infection that has spread and may be life-threatening.
When your jaw makes noises with regular movements it could be a sign of a Temporomandibular Joint disorder or TMJ disorder. TMJ disorders are sometimes difficult to pinpoint and the exact causes are still unknown. What we do know is that signs and symptoms of TMJ disorder include clicking, crunching, and grinding noises emanating from the temporomandibular joint. This is often accompanied by pain, joint discomfort, lockjaw, and swelling.
If you are experiencing these symptoms I recommend you see us as soon as possible to determine an appropriate treatment plan for you.
Dry mouth is a common side effect of many varieties of medicines. It is also a common symptom of oral disease or illnesses.
Medications such as antihistamines, blood pressure medications, painkillers, decongestants, antidepressants, diuretics, and many others have all been implicated in causing dry mouth in people.
Furthermore, many common diseases such as diabetes have also been known to cause dry mouth. Pain, anxiety, and stress are also factors that result in dry mouth.
While it may be difficult to pinpoint the underlying cause of dry mouth, you can be certain that it may be symptomatic of an underlying health issue. I recommend you contact us if you are having these symptoms.